|
The Scenario
You are the nominated “medic” on a voluntary project in Africa (There is no altitude or malarial risk for the group). Your group consists of 24 volunteers roughly split male/female aged between 18 and 63, everyone is in good health with no significant medical or surgical history. You are planning on spending a month on the project. Nearest small rural health centre is 2 days drive away, medivac is possible but would take 24 hours to arrange and get there. All the group have a small personal first aid kit so plenty of plasters, wound dressing and over the counter medication. You have the small medical bag as illustrated approx 35x10x20cm which can contain any equipment or medication you can fit in it. We will assume your competent to use whatever you pack. What would you take ? (Suggestions or complete kit list in comments please)
1 Comment
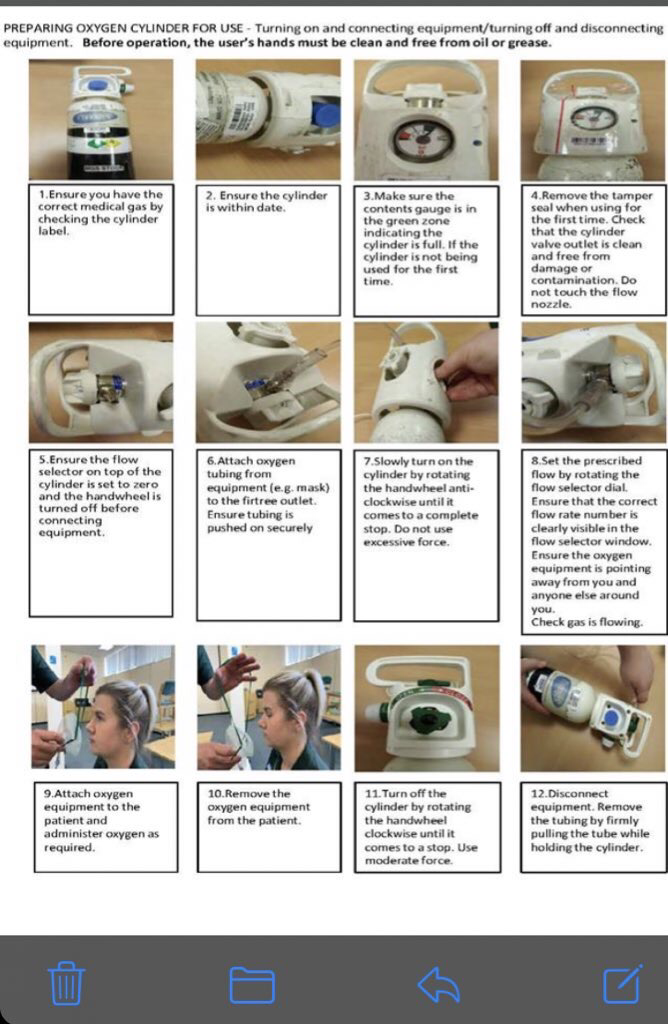
 Picture by James Heilman, MD - Own work, CC BY-SA 3.0 Wound inflammation and Infection Having worked in urgent and emergency medicine I know there is a lot of confusion over inflammation and infection. As many patients presents within 24 hours of receiving a wound believing it is infected. When a wound happens, a healing process starts the first stage of this in inflammation, in the inflammatory stage blood clots and the area around the wound may swell and become surrounded by a red border, as long as that red border remains around the edge of the wound this can usually be attributed to inflammation rather than infection. If the red border starts spreading away from the wound in an irregular pattern, which usually starts around 24-48 hours after the initial wound then this is an indication of infection which is treated with an oral antibiotic such as flucloxacillin or Doxycycline which is covered on and obtainable after our expedition medic course for remote foreign travel. A future point of confusion is when people see fluid leaking from the wound some may automatically think this is pus and therefore a sign of infection, however this is often exudate which is a by-product of wound healing. Exudate being a thin clear liquid whereas pus is a foul thicker liquid. A final sign to look out for is ascending lymphangitis this is a red line moving towards your groin or armpit, this more often occurs on the limbs as illustrated by the picture above but can also appear on the torso. This is a potential life-threatening medial emergency, although they can sometime be treated with oral medication, they often need regular intravenous antibiotics. This condition is also known as blood poisoning although this is inaccurate as the red line, tracing the path of the lymphatic system not the veins. However, if it gets to the glands in the armpit and groin it can enter the blood stream from here and cause a whole body (systemic) infection with fever, potentially leading to sepsis and death. If the wound passes through the inflammatory stage it will enter the stage of proliferation where new tissue growth occurs, then to the maturation stage where the tissue is remodelled and should return t its former state. If the wound it particularly wide and / or not teat or closed correctly then a scar may remain following healing. Pain its assessment and Treatment Many medical problems found in remote medicine have an element of pain attached to them weather through injury or a medial cause such as dental, abdominal and chest pain. Therefore, an understanding of the assessment and treatment of pain is essential When assessing a patient and taking a history, always ask open questions or seek clarification rather than use closed questioning technique. It is well documented that when asking closed questions patients often agree with you even if they are not experiencing what you ask them about. This is because patients often feel that the questioner knows more about the condition than they do and if asked if they suffer a symptom feel they should have it so agree to please the questioner. It is better to ask, “What sort of pain is it” rather than “Is it a crushing pain”. After you have finished asking questions summarise the information and ask if your impression is correct and do, they wish to change or expand on anything. Some patients are very verbose in response to open questioning, so on occasions a mixture may need to be used. If the patient has pain, then this can be assessed using either the OPQRSTA or SOCRATES aide memoires . OPQRSTA (O)nset When did the pain start, what were you doing or had been doing before it started? (P) Provoke, Palliate or Prevent Does anything bring the pain on (Provoke), lessen (Palliate) or prevent it? Pain that is more intense when taking a deep breath is more likely to be caused by problem with the lungs or the muscles between the ribs (Intercostals). But a patient with a constant central chest pain is more likely to have a heart problem. (Q)uality What is the pain like is it sharp, dull, crushing, or tight? Be cautious with this as the patient’s idea of what the pain feels like may not fit with a textbook answer. A person may describe both the discomfort caused by a heart attack and asthma as a heavy pain. But others could separately describe them as crushing and tight. (R)adiation / (R)epeat Does the pain go anywhere else, both chest and abdominal pain can often spread through to the back, arms, neck, and shoulders? In the case of shortness of breath, the ‘R’ for Radiation becomes Repeat i.e. has this happened before and what was the outcome. (S)everity How bad is the pain, is it at a constant level or does it come and go? A good measure is to use a Pain score, ask the patient to set a number against the pain “where zero is no pain and ten is the worst pain they have experienced” again this can be subjective but is a good measure to see if treatment is effective. Score the pain at the beginning and after each intervention that could relieve it. (T)ime How long and how frequent is the pain. (A)ssociated Symptoms Such as nausea or a feeling of doom felt by people having a heart attack. SOCRATES (S)ite Where is the Pain (O)nset When did the pain start, what were you doing or had been doing before it started? (C)haracter What is the pain like is it sharp, dull, crushing, or tight? Be cautious with this as the patient’s idea of what the pain feels like may not fit with a textbook answer. A person may describe both the discomfort caused by a heart attack and asthma as a heavy pain. But others could separately describe them as crushing and tight. (R)adiation Does the pain go anywhere else, both chest and abdominal pain can often spread through to the back, arms, neck and shoulders? In the case of shortness of breath, the ‘R’ for Radiation becomes Repeat i.e. has this happened before and what was the outcome. (A)ssociated Symptoms Such as nausea or a feeling of doom felt by people having a heart attack. (T)ime, How long and how frequent is the pain. (E)xacerbating/relieving factors Does anything bring the pain on (Exacerbating), lessen (relieving) or prevent it? Pain that is more intense when taking a deep breath is more likely to be caused by problem with the lungs or the muscles between the ribs (Intercostals). But a patient with a constant central chest pain is more likely to have a heart problem. (S)everity How bad is the pain, is it at a constant level or does it come and go? A good measure is to use a Pain score, ask the patient to set a number against the pain “where zero is no pain and ten is the worst pain they have experienced” again this can be subjective but is a good measure to see if treatment is effective. Score the pain at the beginning and after each intervention that could relieve it. It’s beyond the scope of this article to discuss all the injuries and problems that can cause pain but some will be covered in future posts. Local anaesthetic Local anaesthetic has many uses in the wilderness setting as it allows the practitioner to deaden an area of the patient’s body which allows painful procedures to be carried out more comfortably. It has advantages over general anaesthetic as the patient does not need to be paralysed or sedated. This will be discussed in a future post Oral. Inhaled and injected Medication The following pain-relieving medication is cover on our Expedition Medicine Courses and is available post course for bulk purchase for remote foreign travel. ASPIRIN SOLUBLE 300MG TABS IBUPROFEN 400MG TABS PARACETAMOL 500MG TABS TETRACAINE 1% DROPS POM for treatment of Eyes CO-CODAMOL 500MG/30MG TABS POM NAPROXEN 500MG TABS POM PENTHROX POM TRAMADOL 50MG CAPS (POM & Schedule 3 CD) TRAMADOL 100MG INJ (POM & Schedule 3 CD) LIDOCAINE 1% 5ML AMPS POM See our Expedition Medicine Courses for further details Safe use of oxygen poster, oxygen and entenox covered on our IPOS, Responder, ILS, PILS and expedition medic courses survivalmedic.co.uk
All schedules dates are now going ahead As of the 1st June amendments to social distancing, now allows up to 6 people to gather outdoors for recreational purposes providing they maintain social distancing, if further states larger groups are permitted for educational purposes. However to keep our staff and customers safe we are keeping to small groups. Further we are encouraging face coverings and will supply PPE (masks and gloves) to clients, hand washing and/or alcohol gel also available. A full guarantee will be given that you won’t lose any money and new dates will be bookable if you are unwell or government guidance changes after booking. All attendees will be screened for covid symptoms, including temperature checks. Disposable and single person items will be used where possible and any shared equipment will be cleaned with alcohol types between and after student use. Training packs of dressings supplied individually which you take away afterwards. If you are looking to book one of our courses book now to avoid disappointment as places will be limited. Expedition Medicine – why?
Standard medical care is based around a functional Ambulance service and ready access to General Practitioners and Hospitals. What if that is no longer the case either through remote foreign travel, disaster, crisis? And why bother if you are not a doctor or paramedic, you may think that its beyond your knowledge and skill A. Medical Care after major disaster or prolonged catastrophe. There is a sense when thinking about survival or disaster medicine practice that everything is overwhelming, that it is impossible for lay people to provide a high level of medical care and maintain a high level of population health. We do not believe this is the case at all. Consider the following: 1. Remote Medicine practice: Below are the results of one author’s experience in the provision of health care in various remote and austere locations (some third world, some first world) to several thousand people over a cumulative 10 years. The Top 20 presentations (representing > 95% of consultations): 1. Minor musculoskeletal injuries (ankle sprains most common) 2. Upper respiratory tract infections 3. Allergic reactions/Hay fever/Anaphylactic reactions/Rashes 4. Minor open wounds 5. Gastroenteritis/Vomiting/Diarrhoea 6. Sexual health/Contraceptive problems 7. Skin infections/Cellulites 8. Mental health problems 9. Dental problems 10. Abdominal pain (2 confirmed acute appendix + 1 gangrenous gall bladder; no cause found. Renal or biliary colic were most common) 11. Flu/Viral illness 12. Chest infections 13. Major musculoskeletal injuries (fractures/dislocations) 14. Asthma 15. Ear infections 16. Urinary tract infections 17. Chest pain 18. Syncope/Collapse/Faints 19. Early pregnancy problems 20. Burns Top 12 prescribed drugs (representing >90% of medications prescribed): 1. Paracetamol (Acetaminophen) 2. Loratadine (and other assorted antihistamines) 3. Diclofenac (and other assorted anti-inflammatory) 4. Combined oral contraceptive 5. Flucloxacillin 6. Throat lozenges 7. Augmentin 8. Loperamide 9. Nystatin (and other antifungal) 10. Hydrocortisone cream 11. Ventolin inhalers 12. Morphine or other strong Analgesia What is of note here is that the vast majority of problems dealt with are simple and straight forward – there is still potential for serious consequences but there is scope for a well-informed lay person with a some training and access to a reasonable collection of reference books to provide reasonable care. Equally the vast majority of medication prescribed are from a very narrow well-defined list – despite the fact 1000’s of drugs that are on the market – the list of core lifesaving or comfort preserving ones is relatively brief. If you want to know more why not check out our expedition medicine courses which provides the necessary training and access to prescription medicines for remote travel. |
AuthorThe author is a Registered Nurse who served with the RAMC, a Paramedic and Clinical Tutor with additional qualifications in Trauma and Remote Medicine. He has had a long term interest in remote medicine and is the Medical Advisor for several groups and runs courses in Outdoor First Aid, Expedition, Remote and Survival Medicine. ArchivesCategories |
- Home
- Upcoming Courses
-
All Courses
- Outdoor First Aid
- Advanced Outdoor First Aid
- Paediatric First Aid Course
- Emergency First Aid at Work (EFAW+F) forestry
- ITC Level 3 Award in Outdoor First Aid
- Immediate Life Support (ILS)
- Expedition Medic
- Remote medical emergencies
- Award in Education and training
- First Person On Scene/Responder Courses
- CPR/BLS For Healthcare professionals
- Pet First Aid
- Mental Health in the Workplace
- Advanced First Aid Courses
- Standard First Aid Courses
- Short First Aid Courses
- Forestry and Outdoor First Aid
- Health and Safety Courses
- Introduction to Infection Control
- Online Dog and Pet Care Courses
- Contact
- Gallery
- Activities
- Products
- Resources
- Online Courses
- Recommended Reading
- Survival Medic Blog
- QUZZES
- Tactical Medical Equipment
- Expedtion Medic Refreshers
- Minor Injury Online
- Expedition Medic Weekend
Location |
|


 RSS Feed
RSS Feed

